Glaucoma Surgery
Most patients with glaucoma in the United States do not require glaucoma surgery. With today’s advanced and early glaucoma detection, eye doctors are now able to stabilize glaucoma sooner without resorting to surgery. However, even with the best care some glaucoma continues to progress. If one’s glaucoma progresses despite using eye drops and laser treatment, glaucoma surgery is sometimes indicated.
The Parschauer Eye Center is fortunate to have doctors on staff at Parschauer Eye Center. Dr. Igor Estrovich and Dr. Alexander Kosmidis are Ophthalmologists who specialize in glaucoma procedures.
There are several different forms of glaucoma surgery that include:
Trabeculectomy
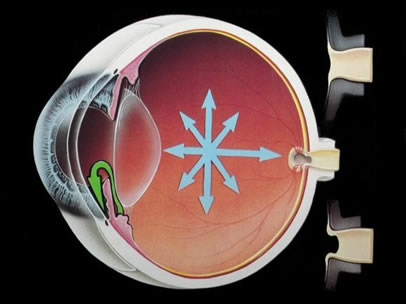
Trabeculectomy surgery creates a “trap door” and an extra pocket so the watery fluid in the eye can escape the eye easier and form a bubble on the eye. This bubble or “bleb” can increase the space within the eye, and therefore, lowers the overall eye pressure. Trabeculectomy is not full-proof and requires a delicate surgeon with excellent working knowledge of the glaucoma disease.
Shunt Procedures
The shunt procedures are a group of surgeries where a tube is inserted into the eye and allows the aqueous or water to flow safely into the blood stream. Once in the eye the shunt can be altered to increase or to decrease the watery outflow.
Cyclo-Destruction
Cyclo-destruction utilizes surgery to partially impair the aqueous or water production system. Cyclo-destruction procedures are reserved for severe or morbid forms of glaucoma where the condition is painful and very progressive.